Scarlet fever is a disease caused by infection with the group A Streptococcus bacteria (the same bacteria that causes strep throat).
Scarlet fever is a disease caused by exotoxin released by Streptococcus pyogenes. Once a major cause of death, it is now effectively treated with antibiotics. The term scarlatina may be used interchangeably with scarlet fever, though it is commonly used to indicate the less acute form of scarlet fever that is often seen since the beginning of the twentieth century.Causes, incidence, and risk factors
Scarlet fever was once a very serious childhood disease, but now is easily treatable. It is caused by the streptococcal bacteria, which produce a toxin that leads to the hallmark red rash of the illness.
The main risk factor is infection with the bacteria that causes strep throat. A history of strep throat or scarlet fever in the community, neighborhood, or school may increase the risk of infection.
Symptoms
The time between becoming infected and having symptoms is short, generally 1 - 2 days. The illness typically begins with a fever and sore throat.
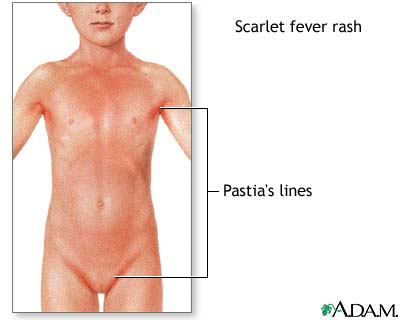
The rash usually first appears on the neck and chest, then spreads over the body. It is described as "sandpapery" in feel. The texture of the rash is more important than the appearance in confirming the diagnosis. The rash can last for more than a week. As the rash fades, peeling (desquamation) may occur around the fingertips, toes, and groin area.
Other symptoms include:
•Abdominal pain
•Bright red color in the creases of the underarm and groin (Pastia's lines)
•Chills
•Fever
•General discomfort (malaise)
•Headache
•Muscle aches
•Sore throat
•Swollen, red tongue (strawberry tongue)
•Vomiting
- is fine, red, and rough-textured; it blanches upon pressure.
- appears 12–48 hours after the fever.
- generally starts on the chest, armpits, and behind the ears.
- spares the face (although some circumoral pallor is characteristic).
- is worse in the skin folds. These Pastia lines (where the rash runs together in the armpits and groin) appear and can persist after the rash is gone.
- may spread to cover the uvula.
- The rash begins to fade three to four days after onset and desquamation (peeling) begins. "This phase begins with flakes peeling from the face. Peeling from the palms and around the fingers occurs about a week later."[3] Peeling also occurs in axilla, groin, and tips of the fingers and toes.
 |
 |
 |
| tongue red as strawberry |
Signs and tests
•Physical examination
•Throat culture positive for group A strep
•Rapid antigen detection (throat swab)
Treatment
Antibiotics are used to kill the bacteria that causes the throat infection. This is crucial to prevent rheumatic fever, a serious complication of strep throat and scarlet fever.
Other than the occurrence of the diarrhea, the treatment and course of scarlet fever are no different from those of any strep throat. In case of penicillin allergy, clindamycin or erythromycin can be used with success. Patients should no longer be infectious after taking antibiotics for 24 hours. People who have been exposed to scarlet fever should be watched carefully for a full week for symptoms, especially if aged 3 to young adult. It is very important to be tested (throat culture) and if positive, seek treatment
Expectations (prognosis)
With proper antibiotic treatment, the symptoms of scarlet fever should get better quickly. However, the rash can last for up to 2 - 3 weeks before it fully goes away.
Complications
Complications are rare with the right treatment, but can include:
•Acute rheumatic fever
•Bone or joint problems (osteomyelitis or arthritis)
•Ear infection (otitis media)
•Inflammation of a gland (adenitis) or abscess
•Kidney damage (glomerulonephritis)
•Liver damage (hepatitis)
•Meningitis
•Pneumonia
•Sinusitis
Calling your health care provider
Call your health care provider if:
•You develop symptoms of scarlet fever
•Your symptoms do not go away 24 hours after beginning antibiotic treatment
•You develop new symptoms
Prevention
Bacteria are spread by direct contact with infected people, or by droplets exhaled by an infected person. Avoid contact with infected people.
History
Husband and wife Gladys Henry Dick and George Frederick Dick developed a vaccine in 1924 that was later eclipsed by penicillin in the 1940s
-------------------------------------------------------
List of cutaneous conditions
From Wikipedia, the free encyclopediaJump to: navigation, search
This is an incomplete list, which may never be able to satisfy particular standards for completeness. You can help by expanding it with reliably sourced entries.
See also: Cutaneous conditions, Category:Cutaneous conditions, and ICD-10 Chapter XII: Diseases of the skin and subcutaneous tissue
MeaslesMany conditions affect the human integumentary system—the organ system covering the entire surface of the body and is composed of skin, hair, nails, and related muscle and glands.[1] The major function of this system is as a barrier against the external environment.[2] The skin weighs an average of four kilograms, covers an area of two square meters, and is made of three distinct layers: the epidermis, dermis, and subcutaneous tissue.[1] There are two main types of human skin: glabrous skin, the nonhairy skin on the palms and soles (also referred to as the "palmoplantar" surfaces), and hair-bearing skin.[3] Within the latter type, there are hairs in structures called pilosebaceous units, each with hair follicle, sebaceous gland, and associated arrector pili muscle.[4] In the embryo, the epidermis, hair, and glands form from the ectoderm, which is chemically influenced by the underlying mesoderm that forms the dermis and subcutaneous tissues.[5][6][7]
 |
| Measles |
The dermis is the layer of skin between the epidermis and subcutaneous tissue, and comprises two sections, the papillary dermis and the reticular dermis.[10] The superficial papillary dermis interdigitates with the overlying rete ridges of the epidermis, between which the two layers interact through the basement membrane zone.[10] Structural components of the dermis are collagen, elastic fibers, and extrafibrillar matrix (previously called ground substance).[10] Within these components are the pilosebaceous units, arrector pili muscles, and the eccrine and apocrine glands.[8] The dermis contains two vascular networks that run parallel to the skin surface—one superficial and one deep plexus—which are connected by vertical communicating vessels.[8][11] The function of blood vessels within the dermis is fourfold: to supply nutrition, to regulate temperature, to modulate inflammation, and to participate in wound healing.[12][13]
The subcutaneous tissue is a layer of fat between the dermis and underlying fascia.[14] This tissue may be further divided into two components, the actual fatty layer, or panniculus adiposus, and a deeper vestigial layer of muscle, the panniculus carnosus.[3] The main cellular component of this tissue is the adipocyte, or fat cell.[14] The structure of this tissue is composed of septal (i.e. linear strands) and lobular compartments, which differ in microscopic appearance.[8] Functionally, the subcutaneous fat insulates the body, absorbs trauma, and serves as a reserve energy source.[14]
Conditions of the human integumentary system constitute a broad spectrum of diseases, also known as dermatoses, as well as many nonpathologic states (like, in certain circumstances, melanonychia and racquet nails).[15][16] While only a small number of skin diseases account for most visits to the physician, thousands of skin conditions have been described.[14] Classification of these conditions often presents many nosological challenges, since underlying etiologies and pathogenetics are often not known.[17][18] Therefore, most current textbooks present a classification based on location (for example, conditions of the mucous membrane), morphology (chronic blistering conditions), etiology (skin conditions resulting from physical factors), and so on.[19][20] Clinically, the diagnosis of any particular skin condition is made by gathering pertinent information regarding the presenting skin lesion(s), including the location (such as arms, head, legs), symptoms (pruritus, pain), duration (acute or chronic), arrangement (solitary, generalized, annular, linear), morphology (macules, papules, vesicles), and color (red, blue, brown, black, white, yellow).[21] The diagnosis of a many conditions often also requires a skin biopsy which yields histologic information[22][23] that can be correlated with the clinical presentation and any laboratory data.[
No comments:
Post a Comment